The fast food-obesity myth
Fast food is high on the ratings scale to explain the modern
epidemic of obesity. It makes sense. These foods are high in calories, high in
fat, highly palatable, cheap, available 24-7, heavily marketed to younger
persons and totally convenient. Moreover, these compelling attributes of guilt
are bolstered by data showing that in the last several decades, the number of fast
food outlets has soared, as have the portion sizes of food they serve. Thus it
is easy to understand why the term ‘fast food’ rolls so easily off the tongue
of policy shapers and makers and why restrictions are called for to limit the
number of fast food outlets and to make fast foods unattractive through higher
taxation and consumer education. But, as Oliver Cromwell said in addressing the
assembled Church of Scotland: “Gentlemen, in the bowels of Christ, I beseech
thee. Think it possible you may be mistaken”. So let us turn to several
recently published scientific articles on this topic.
The first of these
draws on two data sets from the US[1].
The first is county-level data on obesity (BMI>30kg/m2) rates
from the Center for Disease Control and the second is county-level data on both
fast food restaurants (FFRs) and full service restaurants (FSRs) from the US Department
of Agriculture’s economic database. It should be noted that this database lists
not only large chain type FFRs and FSRs but also small local such restaurants.
In all, data was available for the year 2012 involving 3138 counties across the
US involving a population of 170 million. The results were clear cut and expressed
thus by the authors: “Our a priori
prediction that FFRs and FSRs would be positively linked to obesity prevalence
was not supported”. They did find some evidence, which suggested that
such establishments were more likely to be located in areas where there was a
higher level of both income and education.
The authors then pint out that if that is the case, it would make
commercial sense for FFRs and FSRs to be located in more affluent areas and
that given the lower level of obesity with higher income and education, these
outlets were thus located in lower obesity areas. The authors went on to
quantify the extent to which variation in FFRs and FSRs density would explain
variation in obesity, and, controlling for all variables (poverty, ethnicity,
education, employment, household income, local recreational facilities and
health insurance), FFR and FSR density accounted for only 0.8% of obesity. They also calculated that FFR and FSR together
contribute to about a quarter of total US caloric intake.
The second paper
is based on data for 25,000+ European adults, 50 years or older drawing on a
database from the project: ’Survey of Health, Ageing and Retirement in Europe’
(SHARE)[2].
The countries involved are: Denmark, Sweden, Austria, France, Germany,
Switzerland, Belgium, the Netherlands, Spain, Italy and Greece. This survey
measured body mass index and household food expenditure, including expenditure
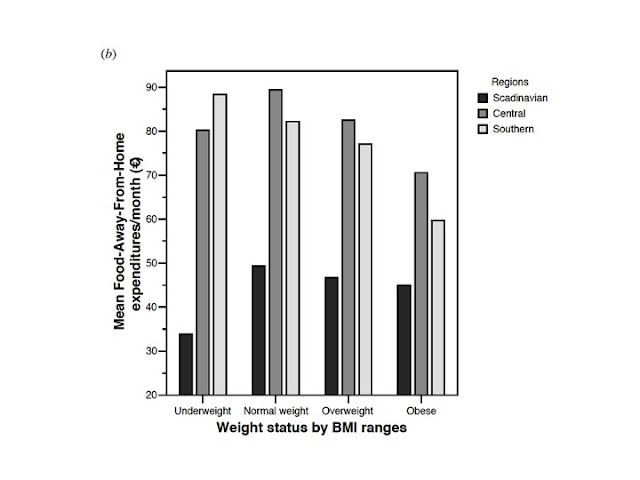
on ‘Food Away From Home” (FAFH). The findings are explained thus by the
authors: ”Our results suggest,
contrary to normative views, that away from home food expenditures negatively
affect BMI and that BMI is negatively related to the percentage of the food
budget spent away from home”. They go on to conclude: “Given our findings, the implication
seems to be that a policy intervention related to the food away from home and
obesity issue is not warranted for older Europeans. But if a policy
prescription is really needed, then a policy that is directed at promoting
better nutritional quality of foods for food-away-from-home might be in order.”
The authors note that these data refer only to older Europeans and may not
apply to younger citizens. The main findings are summarized in Figure 1 below.
Figure 1 from the second study above on the SHARE database of
older Europeans
The third study is
US based and draws on The Coronary Artery Risk Development in Young Adults
(CARDIA) study which in this case involved 12,174 person-observations who participated
in 6 examinations; 1985–2011) across four US cities (Birmingham, AL; Chicago,
IL; Minneapolis, MN; Oakland, CA)[3]. The database was used to provide statistical
input into a variety of models linking the percentage of neighbourhood food
stores or restaurants (per total food outlets within 1 km network distance of
respondent residence) with BMI (kg/m2). The models were adjusted for
socio-demographic and health behaviour data and for city of residence, timing
of subjects examinations, total food outlets and market-level prices. Once
again the findings were clear-cut: “Neighbourhood
convenience stores and fast-food restaurants were not associated with BMI in
any model”.
The fourth and
final study brings us away from out of home food purchases to old-fashioned
home cooked meals[4]. It
recognises that there is ample documentation of the gradual increase in portion
size of foods served outside the home. It then asks the question: Has this also
happened inside the home. The abstract is short and it is worth presenting it
in total: “Since portion sizes have
increased outside the home, could caloric content have increased over the years
within the home? To examine this, a content analysis of common recipes in Better Homes & Gardens, the
bestselling book in its genre, was compared from its first edition in 1930 to
its most recent edition in 2010. Recipes were categorized into appetizers, side
dishes, entrées, and desserts and analyzed for significant changes in total
calories, number of servings, and calories per serving. From its first edition
to its most recent edition, the total calories and calories per serving in
appetizer recipes significantly increased by 51.18% and 52.5%, respectively.
Furthermore, entrée recipes had a significant increase in total calories by
32.96%. As these increases have gone unnoticed for scratch cooks and their
families, cookbook users should be wary of these drastic changes and the amount
consumed to counteract ever-increasing weight gain”.
All of the above suggests that when there is a knee jerk
policy move to curb fast food to reduce obesity, we should absolutely demand
evidence. Certainly the first three studies won’t support this knee jerk
reaction. The fourth is a bit of a shocker since home cooked food has been the ideal
for decades. It is the Walton family shrine of all things wonderful from family
home cooked meals to “Goodnight John Boy”. Sometimes such dreams are shattered.
So we should focus more on the home and ask ourselves how food portion size in
the home (and everywhere else of course) should be reduced. Controlling portion
size was recorded by the McKinsey Global Institute as the top priority for
policy action in tackling obesity. But rest assured, fast food will always be a
handy whipping boy by the evidence-averse mouthpieces of dietary change. Fast food
is s corporate villain but what about my local Chinese or Indian takeaway or my
local fish and chip shop?
[1]
Mazidi m & Speakman JR . Higher densities of
fast-food and full-service restaurants are not associated with obesity
prevalence. American Journal of Clinical Nutrition. May 2017.
[2]
Body Weight Outcomes and Food Expenditures Among
Older Europeans: A simultaneous equation approach Andreas C. Drichoutis1,
Panagiotis Lazaridis2 and Rodolfo M. Nayga, Jr. Paper prepared for presentation
at the 113th EAAE Seminar “A resilient European food industry and food chain in
a challenging world”, Chania, Crete, Greece, date as in: September 3 - 6, 2009
[3].
Rummo PE, Guilkey DK et al. Does unmeasured
confounding influence associations between the retail food environment and body
mass index over time? The Coronary Artery Risk Development in Young Adults
(CARDIA) study. International Journal of Epidemiology, 2017, 1–9 doi:
10.1093/ije/dyx070
[4]
Wansink B & Mukund A. Bigger Homes &
Recipes: How recipe calories have increased over the years FASEB J April 2017
31:957.8